Marijuana and colorectal cancer: Does weed help?



Thirty-seven states across the country have legalized medical marijuana, and approximately 25% - 40% of cancer patients report marijuana usage to relieve or improve their symptoms. What does the research say, and what’s in store for medical marijuana for CRC patients moving forward?
What Is Marijuana?
Marijuana has gone by many names over the years, including weed, pot, bud, ganja, and Mary Jane, to name a few. It comes from the dried flowers of the Cannabis sativa plant and has been used for its therapeutic effects since around 2800 BC.
Marijuana contains more than 100 chemical compounds known as cannabinoids. Cannabinoids interact with our body’s endocannabinoid system (ECS), which controls the learning and memory centers, emotional processing, sleep, temperature control, pain, inflammation, immune response, and appetite. Essentially, the ECS regulates the body’s most crucial functions.
Of these 100+ cannabinoids contained within the marijuana plant, the most commonly known are tetrahydrocannabinol (THC) and cannabinol (CBD). THC is responsible for the psychoactive effects of marijuana – what many term the “high.” Both THC and CBD have been studied for their various therapeutic effects.
It is possible to consume CBD – also known as hemp – as a single compound. CBD has been removed from the federally Controlled Substances Act, and 47 states now allow the sale of hemp-derived CBD products at THC levels of .3% or less. However, this article specifically focuses on the effects of marijuana (which includes THC and CBD) usage among cancer patients, as opposed to CBD usage alone.
How Is Marijuana Consumed?
There are many different ways to consume marijuana, including:
While it is recommended to consult your healthcare provider about your marijuana usage, complications may arise for cancer patients seeking medical advice. A national survey completed in 2021 found that a mere 13% of doctors feel adequately informed to provide cannabis-related recommendations. This is largely due to a lack of training and a need for more clinical studies.
When Is Marijuana Considered Medical, & What Are the Side Effects?
Marijuana is considered medical when it is used to treat or relieve a severe and persisting health condition and prescribed by a licensed doctor in states where it is legal. Each state has its own qualifications, so it is important to check the laws and regulations before pursuing this therapy.
Just like any healthcare option, marijuana is not free from side effects. The most common ones include:
It is best to start with low amounts of THC and go slow when determining if medical marijuana is right for you. Additionally, you should notify your healthcare provider, as it could have an impact on your overall treatment plan or interfere with certain medications.
Marijuana Use and Cancer Symptoms Relief
Despite the risk of side effects, many cancer patients are turning to medical marijuana for symptom relief. Cancer medication, radiation, and chemotherapy are known to cause nausea, neuropathy, vomiting, and pain. Medical marijuana has proven to be an effective tool in addressing many of these complications.
In 2017, the National Academies of Sciences published an evidence-based book, The Health Effects of Cannabis and Cannabinoids. This peer-reviewed body of literature asserts “there is conclusive evidence that oral cannabinoids are effective … in the treatment of chemotherapy-induced nausea and vomiting.”
In addition, the National Cancer Institute, American Cancer Society, and CDC have all noted several studies that show cannabis to be effective at treating nausea and vomiting, pain, neuropathy, anxiety, and sleep.
Anecdotal evidence is also on the rise. In 2018, a study was released that followed 2,970 cancer patients treated with medical marijuana between the years 2015 and 2017. An astounding 95.9% of participants completing the study reported an improvement in their condition with the use of medical marijuana.
Barriers to Medical Marijuana Research
Despite legalization in 37 states and compelling evidence that supports the positive effects of medical marijuana, many barriers still exist. The National Academy of Sciences, National Cancer Institute, American Cancer Society, and CDC all agree that more studies need to be completed to better understand the effects of marijuana as a cancer therapy.
The main challenges researchers face today include:
To overcome these barriers, it is important to continue having conversations about how and why it is necessary to support medical marijuana research, especially in oncology patients. Organizations must work together to end the stigma and put pressure on restrictive federal policies that make research increasingly difficult.
Colorectal Cancer Patients Speak Up About Medical Marijuana
Despite the need for more research, cancer patients are still using this therapy with reported improved outcomes.
“As a patient and now a NED survivor, I researched and discovered real help with small bites of THC edible gummies to deal with side effects like nausea after treatment, peripheral neuropathy pain, and general anxiety. It also helped me with deeper, more healing sleep,” said Howard, a stage IV colon cancer survivor. “Still, it’s important to consult your oncology team and do your research. Not all marijuana and THC is created equal.”
Others share similar experiences.
“I tried THC candy and liquid drops during chemo and radiation to help with my pain and nausea. It wasn’t high doses, but enough to make a difference,” said Sonia, a stage III-C rectal cancer survivor. “It helped control my pain and nausea, increased my appetite, and helped me get some much-needed sleep and rest. I would choose THC over pain medications any day.”
“The pain that cancer causes patients can be unbearable. First, I was trying a combination of various opioids to control my pain with little luck. THC seemed like a better option,” said Michelle, a stage IV colon and rectal cancer survivor. “I chose to try edibles and tinctures. They helped alleviate my pain, nausea, and reduced some of my inflammation. I did notify my team of my pain management decision. Listen to your body and do what’s best for you. THC worked wonders for me and I would choose it again.”
The stigma associated with marijuana usage – even for medical purposes – can play a huge role in people’s willingness to speak up. Sometimes, patients prefer to remain entirely anonymous.
“THC has helped me in so many ways since my cancer diagnosis. I used it to keep nausea at bay and increase my appetite during chemo. After my surgery, I used it for pain relief and it helped me more than the narcotics they prescribed. As a survivor, I now use it for abdominal pain that begins after eating and to assist in falling asleep at night. I am so grateful to live in a state where it is at least legal for medicinal use,” one patient said.
What’s in Store for the Future of Medical Marijuana Usage in CRC?
The Colorectal Cancer Alliance seeks to end this disease in our lifetime and recognizes the need for unique solutions to complex problems.
“We always stand by the research. While there is not yet enough evidence to directly recommend medical marijuana as a treatment option for colorectal cancer patients, we support the need for further research on this topic as we work to support patients with their quality of life,” said David Fenstermacher, the Alliance’s Senior Director of Research & Medical Affairs.
The Alliance looks forward to the promise that new marijuana research brings for colorectal cancer patients. In the meantime, it’s important that we continue to work on destigmatizing the use of medical marijuana and provide support to patients that use it.
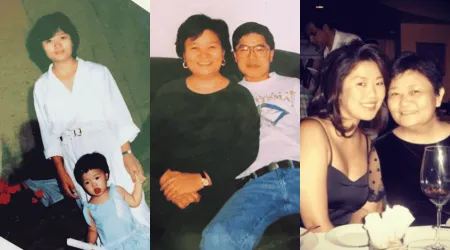
When Kate Shin’s mother faced rectal cancer, clinical trials gave them precious time together. Now, Kate shares her story to encourage access to screening and innovative care, including clinical trials.

Discover hope and healing through Angela and Marleigh Cummins' powerful journey after losing Rodney to colorectal cancer. Learn how their partnership with the Colorectal Cancer Alliance turned grief into advocacy, raising awareness and fostering community support to take on colorectal cancer.

After a stage IV colorectal cancer diagnosis, Heather’s biomarker test revealed a critical mutation — opening the door to clinical trials and new hope.