
Types of colorectal cancer surgery

Surgery is considered the most common treatment for early stage or resectable (removable) colorectal cancers. Doctors will evaluate which type of surgery is best for a patient, depending on the extent of the tumor, where it is located. The three main types of surgery for colorectal cancer are open, laparoscopic, and robotic.
Historically, open surgery for colorectal cancer has been the conventional method for removing tumors. Recent advancements in technology, however, have enabled more laparoscopic and robotic approaches. These are considered minimally invasive surgeries that let doctors make smaller incisions and can decrease recovery time.
A study of more than a million hospitalized colorectal cancer patients showed a 35.4 percent decrease in open surgery between 2004 and 2012, though it remains the most common type of procedure. Laparoscopic surgeries increased more than three times to 31.2 percent, and robotic surgeries increased more than 41 times, though robotic surgeries have the smallest share of operations at 3.4 percent.
The decision to use minimally invasive surgery or open surgery should be discussed with a patient’s healthcare team. Which type of operation is better for the patient is dependent on numerous factors, including the surgeon’s experience and a patient’s health. Open surgeries can take less time than minimally invasive surgeries, but minimally invasive surgeries usually have a faster recovery time. The type of anesthesia and sedation required for each varies.
Laparoscopic surgery (minimally invasive)
Laparoscopic surgery is a specialized minimally invasive surgery in which the surgeon uses several small abdominal incisions (0.5-1 cm) to insert surgical instruments into the abdominal cavity as well as a long thin lighted tube with a camera on the end called laparoscope. A larger incision, about 3 cm wide, is made to remove the tumor. The laparoscope transmits images from the abdominal cavity to high-resolution video monitors in the operating room. The surgical instruments function as an extension of the surgeon's hands to dissect and resect the tumor. During the operation, the surgeon observes the abdomen and manipulates the instruments by watching the monitors. The resected tumor is removed through the larger incision.

Robotic surgery (minimally invasive)
The first robotic colorectal surgery was performed in 2001. Robotic surgery lets surgeons use miniaturized instruments, operated with a console, and a 3D camera to complete an operation from a comfortable seated position with enhanced precision, flexibility, and control. The surgical instruments are inserted through small incisions and remain under full control of the surgeon. Robotic surgery comes at a high cost and may be used in conjunction with laparoscopic methods. Minimally invasive rectal cancer surgeries are often completed robotically.

Open surgery
During open surgery, the surgeon makes a large cut into the abdomen to remove the tumor and part of the healthy colon or rectum. Some nearby lymph nodes are also removed. The surgeon will check the rest of the intestines and liver to see if the cancer has spread. The large incisions affect recovery time.

Types of colorectal cancer resection surgeries
Separate from the method by which a surgeon completes a procedure, there are many types of operations. The specific type of surgery is determined by the location of the disease. Four common types are right hemicolectomy, sigmoid colectomy, left hemicolectomy, and lower anterior resection (LAR).
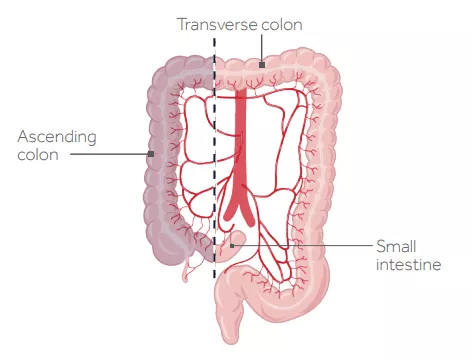
Right hemicolectomy
The surgeon removes the ascending colon and a portion of the transverse colon and then connects the transverse colon to the end of the small intestine. Most patients gain bowel function within 3 days after surgery. Patients who had a right hemicolectomy surgery may experience a slower return of bowel function, which will cause a longer stay at the hospital.
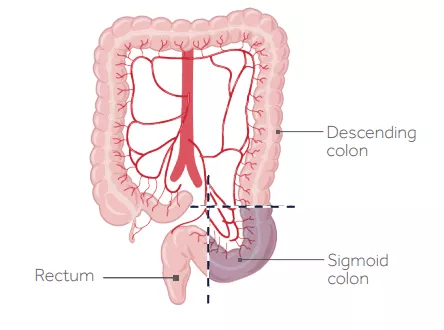
Sigmoid colectomy
The surgeon removes the diseased portion of the sigmoid colon and then connects the descending colon to the rectum.
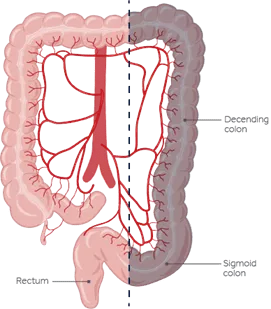
Left hemicolectomy
The surgeon removes a portion of the transverse colon, the descending colon, and the sigmoid colon and then connects the transverse colon to the rectum. With this surgery, patients may have an increased risk of infections at the site of surgery. Surgeons are more likely to create a temporary ostomy in patients who had left hemicolectomy, which may extend their stay at the hospital.
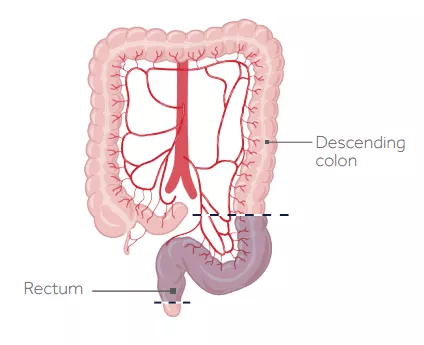
Lower anterior resection (LAR)
The surgeon removes the diseased portion of the rectum and then reconnects it to the descending colon. With this type of surgery patients are at higher risk of a leak from the site of reattachment of the health ends of the rectum (anastomotic leak) and fecal incontinence. To reduce the risk, your surgeon may create a temporary ostomy to divert fecal matter away from the newly created anastomosis. Rectal cancer patients are also at increased risk of developing LARS syndrome (a collection of symptoms ranging from incontinence with frequency and urgency to constipation and incomplete emptying) following their surgery. Patients who had a lower anterior resection are more likely to suffer from sexual dysfunction.
Before and after surgery
Patients are encouraged to discuss surgical options with their medical teams, along with details about surgery preparation and recovery. Surgery must be conducted on a clean and empty colon, which is achieved through preparation like the one used before a colonoscopy. Patients do face possible risks and side effects during or shortly after surgery, such as bleeding, infection, and blood clots in the legs. Immediately after surgery, patients can expect pain, which can be managed with medicine. Most patients are able to eat solid food within a few days. Thousands go on to live happy and productive lives.
Learn more in this video from Medtronic

Top resources
"Clinical trials gave us time": A daughter’s tribute to her mother’s courage
When Kate Shin’s mother faced rectal cancer, clinical trials gave them precious time together. Now, Kate shares her story to encourage access to screening and innovative care, including clinical trials.

2025 ASCO update: Six big studies
The 2025 ASCO Annual Meeting featured several important studies that could change how colorectal cancer is treated, including a pivotal study for BRAF V600E patients.

Hope in the Details: How Heather’s Biomarker Opened New Treatment Paths
After a stage IV colorectal cancer diagnosis, Heather’s biomarker test revealed a critical mutation — opening the door to clinical trials and new hope.





